In peripheral arterial disease (PAD), which is often referred to as peripheral vascular disease (PVD) narrowed or blocked blood vessels in the legs result in reduced blood flow to both the feet and legs. This can produce a range of consequences for the feet as the cells and tissues suffer, hence those diagnosed with PAD and other blood flow impairments to the feet must take special precautions to look after their feet, maintain their foot health, and prevent serious problems like foot ulcers.

PAD: The low-down
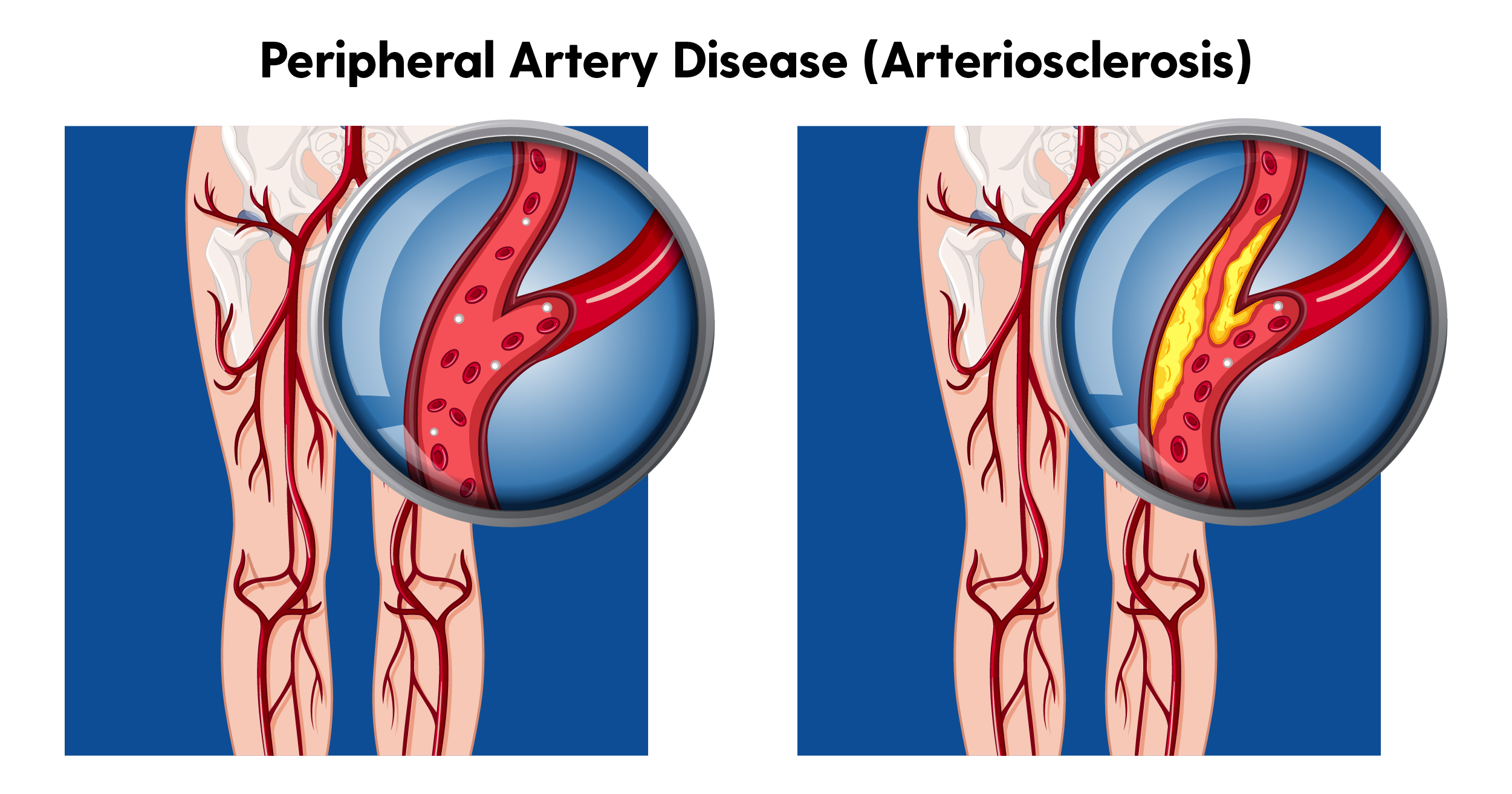
A gradual build-up of plaque on the inner walls of the arteries obstruct regular, healthy volumes of blood from passing through at an adequate rate to get to the tissues of the feet. This plaque is composed primarily of cholesterol and calcium, and those with high cholesterol levels, that smoke, or who have diabetes are most at risk of PAD.
As PAD may not have any notable symptoms in the early stages, it is often picked up by checking blood cholesterol levels and then with explorative arterial studies or imaging. Aside from the consequences on the feet, PAD significantly increases your risk of suffering a heart attack and stroke. While PAD is uncommon in young adults, over 22% of those aged 75+ years currently have a PAD diagnosis.
The Risks For The Feet And Legs
Without an adequate blood supply to the feet and legs, the cells and tissues don’t receive sufficient oxygen, nutrients or energy for healthy function. As a result, you may experience:
Intermittent claudication
Intermittent claudication describes muscle pain and cramping in the feet and legs during exercise, whether it be strenuous activity or simple walking. It often affects the calves, and often starts as a niggle or ache before progressing to cripling, limping pain. This is usually the earliest and most common PAD symptom.
Slower to heal wounds and injuries
When we have a wound or an injury, our body and cells require a healthy blood supply in order to effectively repair, heal and close the wound. This means that both wounds and injuries heal slower with PAD, causing painful symptoms for longer and increasing the risk of complications for our feet.
Increased infection risk
The slower wounds heal, the longer they stay open and are susceptible to infection. If an infection does take hold, the diminished blood flow will also make it harder for the body to effectively fight and clear the infection.
Ischaemia
In less common but more severe cases, a person may develop a sudden and serious restriction in blood flow which may cause tissue death or paralysis. This can put you at risk of limb loss, and requires urgent medical attention.
Other problems that occur in the feet and legs as a result of PAD include:
- Cold feet and toes
- Pale or purple skin discolouration
- Weakness in the legs and feet
- Tired, achy legs
- Problems with gait or balance
- Foot and leg pain
- Numbness and tingling
Your Podiatrist Plays A Crucial Role
As podiatrists, we can pick up on the early warning signs of PAD by examining your arterial pulses at the tops of your feet and around your ankles. We’ll also look for other signs of diminished blood flow to the feet including your capillary refill time (CRT), hair growth (or the absence of) around your toes, the colour and texture of the skin on the feet, or performing an ankle-brachial index (ABI) test.
Using these results, we’ll fill your GP in on the results, refer you appropriately if required, and discuss how you can best look after your foot health.
Managing The Effects Of PAD On The Feet
While there are a number of general things you can do to minimise the impact of PAD, like ceasing smoking, lowering your cholesterol, eating well, exercising, reducing stress and taking certain medications. There are also a number of extra steps you can take to care for your foot health specifically and manage the risks we mentioned above. These include:
- Check your feet and legs regularly for any new cuts or wounds. Take note of when they appear, and how long it takes for them to close. If you do not see any signs of healing after three days, inform your GP
- Monitor any wounds or abrasions for signs of infection. If an infection develops, inform your GP immediately. Signs of infection include increasing redness or swelling around the wound, increasing pain, yellow-green or cloudy discharge and fever
- Keep your feet protected with the right shoes to prevent wounds before they start. Easy ways to do this include avoiding walking with bare feet, swapping thongs for enclosed footwear, and making sure your existing footwear isn’t causing rubbing or blistering
- Manage existing foot problems. Problems like cracked heels, soft corns and skin macerations all serve as a potential entry point for infection-causing bacteria and require effective healing from your body. Working to manage these or prevent them occurring can help you avoid serious consequences for your feet





